Based on what I’ve read on the corona virus in the last two days, the situation is far more dangerous than we have realized. In short: we should minimize the number of people we spend time with to avoid massive death counts this spring. Start working remotely if at all possible. Here’s why.
- Covid-19 aka. the corona virus is extremely contagious. “The number of people found to be infected with covid-19 doubles every 3 to 6 days.” This means the potential of a 100-fold increase in infections in three weeks if we don’t take strong measures to limit its spread.
- You can get an infection from breathing the same air with an infected person or touching them. As some people still have the habit of sneezing into their palms, it may be possible to get an infection from touching something an infected person touched recently, such as a door handle or a food ladle in a lunch buffet.
- You have no way to tell whether you or someone else is already infected, short from doing a full test. Covid-19 is transmissible before symptoms appear.
- The disease is over 30 times more deadly than a seasonal flu, even when people have access to intensive care in a hospital (extra oxygen etc.).
- Approximately 10% of the infected need intensive hospital care for 3-6 weeks.
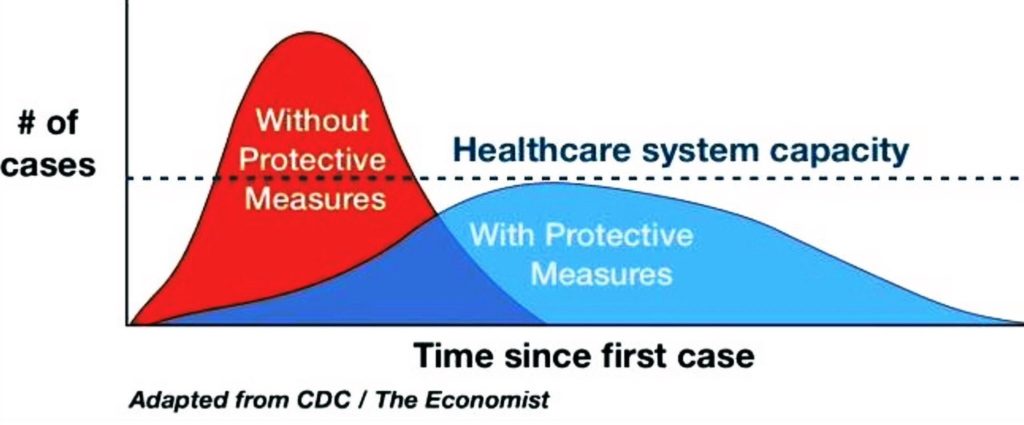
- Because of the high infection rate, hospitals run out of capacity fast. People will start dying from more causes than just covid-19 if we run out of doctors and nurses to perform urgent heart surgeries and other operations. Northern Italy went from zero to that in three weeks.
- Most of the infected people have mild symptoms or none at all. They will still infect other people if they continue business as usual.
This is all based on what we know of the situation as of this morning. New information comes in daily, but we’ve already reached the point where we need to take significant actions to avoid further catastrophes like in Northern Italy, Iran and Wuhan. The numbers on confirmed cases of infection lead to a false sense of security. Regardless of whether we have 2 or 2,000 infections so far, the real question is who did the infected ones spend time with in the last two weeks? And in turn, who did those people spend time with?
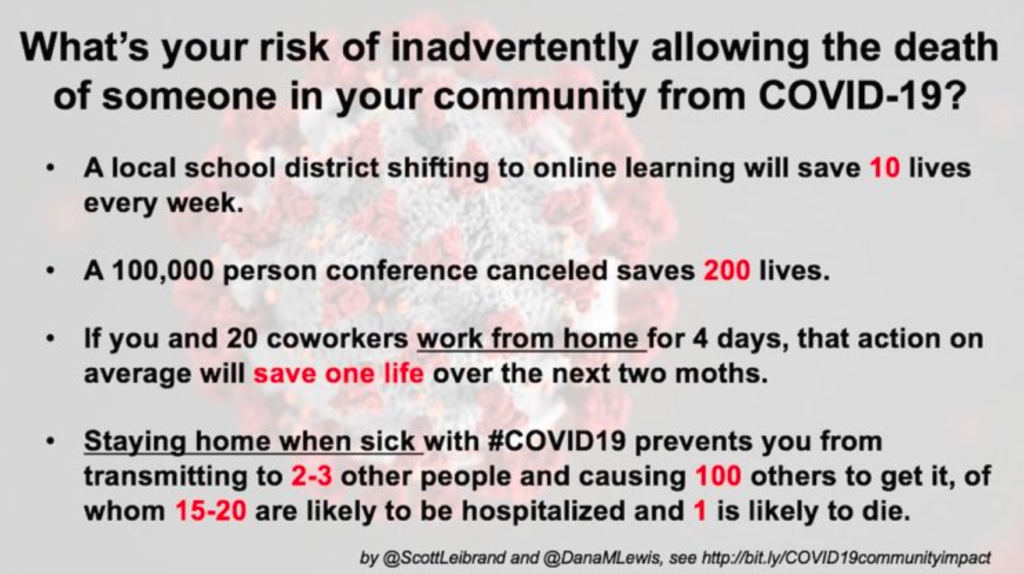
If an infected person attended a 100 person event, and several other participants attended other 100 person events next week, the number of infections may have just grown hundredfold in a week before anyone developed any symptoms. Many cafeterias have anywhere from 15 to 150 people eating lunch at the same closed space for 30-60 minutes. Team meetings may have a dozen people sitting in the same small room for more than an hour. Traveling puts groups of people in the same closed space for hours at a time.
As we have no way of knowing who’s infected, or whether we have been infected ourselves, the safe course of action is to minimize the number of people you spend time with in closed spaces. The virus lives as long as it can infect new people. We can kill it by starving it of opportunities to spread.
We can react either early or too late.
Sources and more information
Michael Osterholm’s explanation was instrumental in helping me understand that covid-19 is not just serious, it’s deadly serious. It may cause a cascade of horrible effects like running out of life-critical medicines if we don’t act quickly. The delayed responses so far have caused us to fail to prevent it from becoming a pandemic, but we can still prevent countless deaths by acting quickly and decisively.
A second, shorter clip answers questions like why hand sanitizing and surgical face masks are helpful but far from enough:
A doctor in Northern Italy describes how they fail to keep many people alive because the number of patients far exceeds the capacity of the medical staff. People are dying from more causes than just covid-19 as there just aren’t enough doctors, nurses and premises to provide life-critical care for everyone. https://threadreaderapp.com/thread/1237142891077697538.html
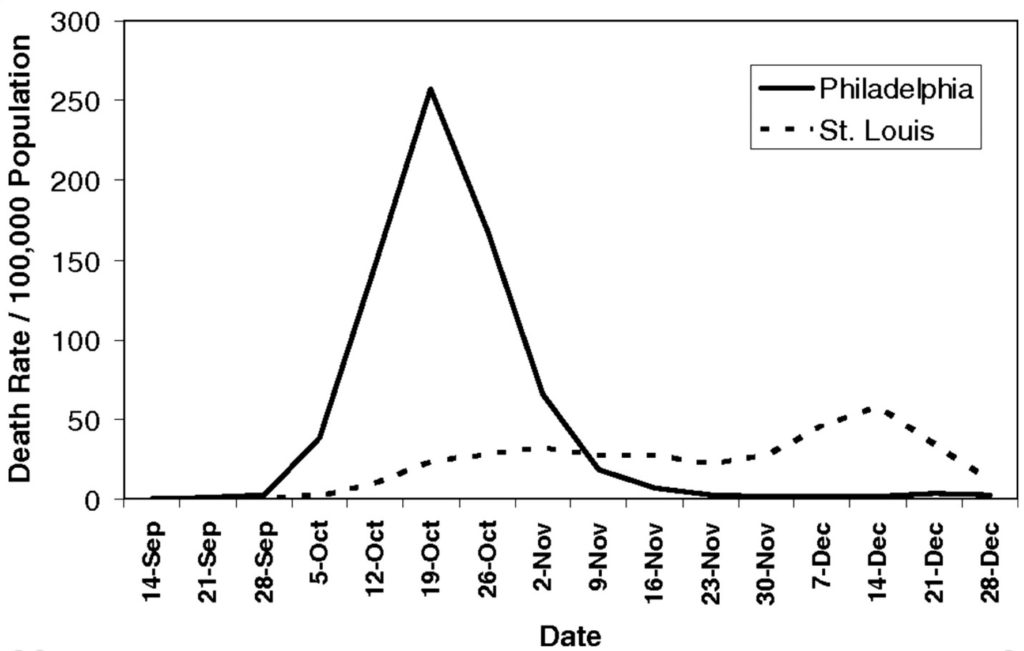
Why community reaction makes all the difference: https://www.fast.ai/2020/03/09/coronavirus/. For example, compare the results of St. Louis’s swift and decisive response with those of the “business as usual” approach of Philadelphia at the outset of the flu pandemic of 1918:
Practical measures to take: https://www.flattenthecurve.com/. This guide is continuously updated.
Questions & Answers
How does the disease spread, precisely?
I haven’t seen a confirmation yet, but it seems likely that it’s transmitted through droplets. The air we exhale is full of tiny droplets of liquid. Because the virus lives in our lungs and throats, it’ll be attached to these droplets. These droplets are exhaled through our mouths and noses and will end up anywhere we are facing for up to almost 2 meters (6 feet). When we sneeze, these can travel much faster. The virus will end up anywhere we breathe on: keyboards and keypads, door handles, buttons, everywhere. We don’t generally pay attention where we breathe to, and even if we did, air currents like ventilation can make it impossible to see where the invisibly small droplets we exhale really end up on.
The air we exhale goes through our noses and mouths and ends up anywhere near them. Our noses are pointed directly at our upper lip to start with. We also touch our faces surprisingly often without noticing it, 20 times an hour according to some studies. As a result our hands are like a train station for viruses, letting viruses transmit to everywhere we touch. We don’t know how long does the virus survive on surfaces, so the safe option right now is to minimize touching items that have been touched or breathed upon recently. Even if the virus survives only 5 minutes on a surface, that’s plenty of time for people to touch the same door handles or elevator buttons as the previous person.
In short, if we inhale the air someone else just exhaled, or touch anything someone touched or breathed on recently, we may get infected. The safe approach is to minimize spending time in the same space as other people until we know for sure what exactly is safe and what isn’t.
Will face masks help?
It seems likely that they do help, especially when worn by people who are infected. The same applies to not just covid-19 but all infectious diseases residing in lungs, throats or mouths and transmitted through droplets or air. A surgical mask aka. “the basic face mask” was made to prevent saliva and droplets from going from medical staff’s mouth and noses into the open wounds of surgery patients. The smallest droplets may go through, and air still goes around the sides, but they seem to significantly decrease the number of droplets transmitted from the wearer to other people and surfaces.
Surgical masks get wet over extended use, and you should avoid touching the wet parts or wash your hands thoroughly right after you do. There are early indications that extensive use of surgical masks may be one of the reasons why Taiwan was one of the best countries in limiting the spread of the disease.
Surgical masks seem extremely underutilized and misunderstood outside Asia. We might have a lot less influenza and common cold cases if people started wearing surgical masks in public when they have flu symptoms. Last year there were 34 million cases and 20 000 deaths from these causes in the US alone, with many people losing a month of productive and happy time to these illnesses. This coronavirus pandemic is a good wake-up call to improve our best practices in limiting the spread of all kinds of respiratory infections.
What’s the purpose of this blog post?
It’s a personal summary for myself and people I interact with to speed up conversations. I spent hours reading on the topic and this was the most efficient way to communicate the key findings to other people.
It might be self-evident, but just to be extra clear, this is not anyone’s official view and nothing here is in any way final. New and better information will arrive in due time and likely significantly change some parts on what we’ve thought until that point.